The Agony of the First Step: A Deep Dive into Plantar Fasciitis
June 16 2025
Stepping out of bed shouldn’t feel like stepping on LEGOs! Our latest article dives deep into plantar fasciitis, uncovering the causes, symptoms, and podiatrist-approved tips to ditch that debilitating heel pain and get you back on your feet.
As a podiatrist, few conditions walk through my door with the consistent regularity, and frankly, the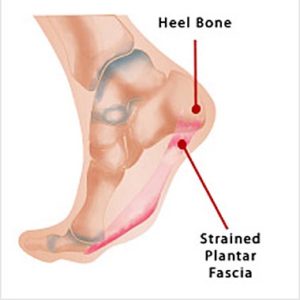 consistent groan, of plantar fasciitis. It’s a common complaint, often uttered with a wince as patients describe that excruciating first step out of bed in the morning, or the sharp, stabbing pain after a period of rest. While not life-threatening, plantar fasciitis can be life-altering, severely impacting daily activities, exercise routines, and overall quality of life. Let’s unravel the mysteries of this ubiquitous heel pain from my perspective in the trenches.
consistent groan, of plantar fasciitis. It’s a common complaint, often uttered with a wince as patients describe that excruciating first step out of bed in the morning, or the sharp, stabbing pain after a period of rest. While not life-threatening, plantar fasciitis can be life-altering, severely impacting daily activities, exercise routines, and overall quality of life. Let’s unravel the mysteries of this ubiquitous heel pain from my perspective in the trenches.
At its core, plantar fasciitis is an inflammation of the plantar fascia – a thick, fibrous band of tissue that runs along the bottom of the foot, connecting the heel bone (calcaneous) to the toes. Think of it as a crucial shock absorber and support structure for the arch of your foot. Every step you take, every jump, every run, places tension on this band. When that tension becomes excessive or repetitive, tiny tears can develop, leading to irritation, inflammation, and the characteristic pain.
So, what exactly triggers this relentless pain? In my experience, a confluence of factors often contributes to the development of plantar fasciitis.
Overuse and Biomechanical Stress
This is perhaps the most significant culprit. Activities that involve repetitive impact, such as running, walking long distances, or standing for prolonged periods, place significant strain on the plantar fascia. Is see it frequently in athletes, especially runners who increase their mileage too quickly, or individuals whose jobs require them to be on their feet all day. Similarly, changes in activity level – say, going from a sedentary lifestyle to suddenly embarking on a vigorous walking program – can shock the fascia.
FOOT STRUCTURE
The architecture of your foot plays a surprisingly large role. Individuals with very high arches (pes cavus) or very flat feet (pes planus) are often more prone to plantar fasciitis. In high arches, the fascia is inherently tighter and under more constant tension. In flat feet, the arch collapses, stretching the fascia excessively. My examination often involves assessing foot type to understand the underlying biomechanical stresses at play.
or very flat feet (pes planus) are often more prone to plantar fasciitis. In high arches, the fascia is inherently tighter and under more constant tension. In flat feet, the arch collapses, stretching the fascia excessively. My examination often involves assessing foot type to understand the underlying biomechanical stresses at play.
IMPROPER FOOTWEAR
This is a surprisingly common, yet easily rectifiable, cause. Worn-out shoes that lack adequate arch support and cushioning or shoes that are too flat, can exacerbate the problem. Many of my patients are surprised to learn that their favorite pair of well-loved, but structurally compromised, sneakers might be contributing to their pain.
TIGHT CALF MUSCLE AND ACHILLES TENDON
This is a crucial, often overlooked, factor. A tight Achilles tendon and calf muscles can limit the ankle’s range of motion. When the ankle can’t adequately dorsiflex (move the foot upwards), the body compensates by overstretching the plantar fascia, leading to increased strain. I always incorporate calf and Achilles stretches into my treatment plans.
WEIGHT
Excess body weight puts additional stress on the plantar, increasing the load it has to bear with every step. Losing even a modest amount of weight can significantly alleviate symptoms for some patients.
The symptoms are typically unmistakable. The hallmark is the post-static dyskinesia – that sharp, burning, or stabbing pain with the first steps in the morning or after prolonged sitting. As the day progresses and the fascia “warms up”, the pain may lessen, only to return with renewed vigor after periods of inactivity. Tenderness along the bottom of the heel, especially towards the inside, is also a classic sign.
When a patient presents with these symptoms, my approach is multifaceted, focusing on conservative, non-surgical treatments first, which are successful in the vast majority of cases.
Rest and Activity Modification: Reducing or temporarily stopping activities that aggravate the pain is crucial. Sometimes, a change to lower-impact exercises like swimming or cycling is recommended.
Ice Therapy: Applying ice to the affected area for 15-20 minutes several times a day can help reduce inflammation and pain.
Stretching Exercises: This is non-negotiable. Specific stretches for t he plantar fascia itself, as well as the calf muscles and Achilles tendon, are vital for long-term relief. I often demonstrate these in the office to ensure proper technique.
Supportive Footwear and Orthotics: I cannot stress enough the importance of good shoes with proper arch support and cushioning. For many, over-the-counter arch supports or custom orthotics can provide the necessary stability and shock absorption to offload the plantar fascia.
Anti-inflammatory Medications: Over-the-counter NSAIDs (non-steroidal anti-inflammatory drugs) can help manage pain and inflammation. In some cases, a short course of prescription anti-inflammatories may be considered.
Corticosteroid Injections: For more severe or persistent cases, a corticosteroid injection into the plantar fascia can provide temporary relief from pain and inflammation. However, this is not a first-line treatment and is used judiciously due to potential risks if overused.
Physical Therapy: A structured physical therapy program can be invaluable, incorporating manuel therapy, strengthening exercises, and advanced stretching techniques.
While surgery is a rare last resort, it is considered only after extensive conservative treatment has failed for at least six to twelve months. Procedures typically involve releasing a portion of the plantar fascia to relieve tension.
The good news? The vast majority of plantar fasciitis cases resolve with consistent, conservative care. It  takes patience and diligence, as the healing process can be gradual. My message to patients is always: listen to your body, be proactive with your self-care, and don’t hesitate to seek professional help. Your feet carry you through life, and keeping your plantar fascia happy is key to keeping you moving without that dreadful first-step agony.
takes patience and diligence, as the healing process can be gradual. My message to patients is always: listen to your body, be proactive with your self-care, and don’t hesitate to seek professional help. Your feet carry you through life, and keeping your plantar fascia happy is key to keeping you moving without that dreadful first-step agony.
If you are experiencing difficult to heal wounds, please contact Dr. Chapman’s office immediately at (239) 430-3668 (FOOT) or visit www.NaplesPodiatrist.com to schedule an examination.
Serving Southwest Florida Since 2005, Family Foot & Leg Center has 9 convenient locations throughout Collier, Lee, Charlotte, and Sarasota Counties. Offering pediatric to geriatric family care: Ingrown Toenails, Heel Pain, Bunions, Foot / Ankle Arthritis Pain, Plantar Fasciitis, Foot / Ankle Surgery, Custom Orthotics, and Diabetic Wound Care. In office X-rays, ultrasounds, and minor surgical suite exam rooms. Practice powered by EMR and advanced technologies.
Home of the Lam Minimally Invasive No-Scar Bunion Surgery! Come Discover Why Patients Love Our 5-Star Foot & Ankle Care!
Same Day Appointments! Easy Online Appointment Scheduling.

 Fax: (239) 692-9436
Fax: (239) 692-9436 Tel: 239-430-3668
Tel: 239-430-3668