A Podiatrist’s Perspective on Morton’s Neuroma
October 10 2025
Feeling like you’re walking on marble? That sharp, burning pain in the ball of your foot could be a neuroma (pinched nerve)! Don’t suffer in silence – early treatment from a Podiatrist means less pain and a better chance to avoid surgery. Get back to pain-free steps! Schedule a check-up!

As a podiatrist, one of the most common and often painful conditions I diagnose and treat is neuroma, frequently referred to by patients as a “pinched nerve” in the foot. While the layman’s term is descriptive of the discomfort – a sharp, shooting, or burning pain often localized to the ball of the foot – a neuroma is actually a specific pathology. It is a benign growth of nerve tissue that develops most often in the forefoot, specifically the area between the metatarsal heads. The most common site is between the third and fourth toes, a condition uniquely and specifically known as Morton’s neuroma. This name is used to honor Thomas G. Morton, who described the condition in 1876.
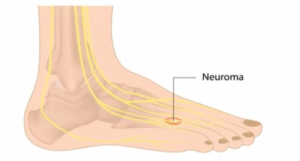
This condition isn’t a true cancerous tumor but rather a thickening and scarring of the nerve sheath and surrounding tissue. This nerve enlargement develops in response to chronic irritation, repetitive pressure, or trauma. Essentially, the smaller plantar nerve becomes chronically compressed and inflamed as it passes under the ligament connecting the metatarsal bones. It’s an inflammatory and mechanical process where the nerve becomes trapped and enlarged, leading to significant symptoms that can severely impact a person’s quality of life and mobility, making activities like walking or standing unbearable. Understanding this precise mechanism is key to effective podiatric management.
Understanding the Symptoms and Causes
The classic presentation of a neuroma often includes a sharp, burning pain in the ball of the foot, which can radiate into the toes. Patients frequently describe the sensation as feeling like they are walking on a marble or a crumpled sock. Other common complaints include tingling (paresthesia), numbness in the toes, and a need to remove the shoe and massage the foot for relief. The pain is typically exacerbated by wearing tight, narrow, or high-heeled shoes, as these shoe types force the metatarsal bones together, increasing the compression on the nerve.
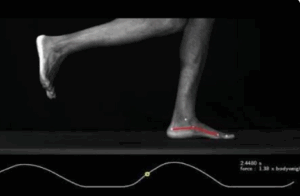
Neuromas are most prevalent in women, likely due to their footwear choices. However, they can also affect athletes whose activities, such as running or racquet sports, place repetitive stress and pressure on the forefoot. Biomechanical factors like flat feet or high arches, as well as foot deformities like bunions or hammertoes, can also contribute to the development of a neuroma by altering the foot’s mechanics and increasing instability and pressure on the intermetatarsal nerves.
The Podiatric Diagnosis
Diagnosis begins with a thorough patient history to understand the nature and location of the pain. I then perform a physical examination of the foot. A key diagnostic sign is the ability to reproduce the symptoms by squeezing the forefoot (the Mulder’s click test). This maneuver compresses the metatarsal heads, causing the neuroma to move and click, often recreating the patient’s characteristic sharp pain.
 While the clinical exam is usually sufficient, imaging studies are often used to confirm the diagnosis or rule out other conditions like a stress fracture or synovitis. Ultrasound is a non-invasive and highly effective tool for visualizing the soft tissues and confirming the size and location of the neuroma. In some cases, an MRI may be ordered, though it is usually reserved for more complex diagnoses.
While the clinical exam is usually sufficient, imaging studies are often used to confirm the diagnosis or rule out other conditions like a stress fracture or synovitis. Ultrasound is a non-invasive and highly effective tool for visualizing the soft tissues and confirming the size and location of the neuroma. In some cases, an MRI may be ordered, though it is usually reserved for more complex diagnoses.
Conservative Treatment: The Initial Approach
As a podiatrist, my treatment philosophy always starts with the most conservative, non-invasive methods possible. The goal of early treatment is to decompress the nerve, reduce inflammation, and alleviate symptoms.
- Footwear ModificationThe simplest and most critical step is a change in footwear. I strongly advise patients to switch to low-heeled shoes with a wide toe box to allow the metatarsal bones to spread out, thereby reducing pressure on the nerve. Avoiding high heels and narrow, pointy-toed shoes is essential for symptom relief.
- Custom Orthotics and Padding Custom functional orthotics are invaluable. These are prescription medical devices tailored to the patient’s specific foot structure. They work by addressing underlying biomechanical issues and providing a metatarsal pad – a teardrop-shaped piece of padding strategically placed just behind the affected metatarsal heads. This pad helps to separate the bones and lift the metatarsals, relieving pressure and splaying the toes to give the nerve more space.
- Anti-inflammatory Medication Over-the-Counter Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), such as ibuprofen, can help reduce pain and inflammation associated with the nerve irritation.
- Corticosteroid InjectionsIf conservative measures fail to provide relief, corticosteroid injections are often the next step. A mixture of a local anesthetic and a strong anti-inflammatory steroid is injected directly into the area of the neuroma. This provides powerful localized relief by reducing the swelling around the nerve. While highly effective, these injections are typically limited to two or three per year to prevent soft tissue damage.
- Alcohol Sclerosing Injections (Chemical Neurolysis)In cases where steroids provide only temporary relief, I may recommend a series of alcohol sclerosing injections. These are high-concentration alcohol solutions injected directly into the neuroma. The alcohol acts as a neurolytic agent, intentionally causing a chemical breakdown of the nerve’s outer sheath, which gradually “deadens” the nerve and stops it from transmitting pain signals. This technique has a high success rate and avoids surgery, though it typically requires multiple sessions.
Surgical Intervention: When Conservative Care Fails
When all conservative and minimally invasive treatments fail to resolve the pain after several months, surgical intervention becomes a necessary discussion. The patient’s quality of life and persistent pain are the determining factors.
The most common procedure is a neurectomy, which involves the surgical removal of the painful neuroma. The procedure is usually performed throug a small incision on the top (dorsal) or bottom (plantar) of the foot.
- Dorsal Incision
- Plantar IncisionA plantar (bottom-of-the-foot) approach may be necessary for very large or recurrent neuromas, though it carries a slightly higher risk of a painful scar upon walking. In rare instances, or for patients with very significant foot instability contributing to the neuroma, a procedure to decompress the nerve without removing it, or an accompanying metatarsal shortening osteotomy to change the foot’s mechanics, may be considered.
Following a neurectomy, patients can expect a period of post-operative recovery, typically involving a surgical shoe, limited weight-bearing, and physical therapy. While surgery offers a high success rate, it does result in permanent numbness in the affected toes, a trade-off that is usually well worth the elimination of the sharp, chronic pain.
At Family Foot & Leg Center, a neuroma is a condition that demands careful and progressive  management. With accurate diagnosis and a tailored treatment plan – starting with footwear modifications and progressing through injections and, if necessary, surgery – patients can effectively be relieved of this frustrating and debilitating “pinched nerve” and return to pain-free activity.
management. With accurate diagnosis and a tailored treatment plan – starting with footwear modifications and progressing through injections and, if necessary, surgery – patients can effectively be relieved of this frustrating and debilitating “pinched nerve” and return to pain-free activity.
If you’ve been experiencing the tell-tale sharp, burning pain in the ball of your foot or feel like you’re constantly walking on a marble, don’t dismiss it as just a temporary ache. Chronic neuroma pain will not resolve on its own and often worsens without professional intervention. The sooner we identify the issue and begin treatment, the more likely we are to find relief through non-surgical methods. Don’t let a “pinched nerve” dictate your mobility or your shoe choices. Take the first step toward reclaiming comfortable, pain-free walking by scheduling a comprehensive foot examination with a podiatrist today.
If you are experiencing neuroma symptoms, please contact Dr. Chapman’s office immediately at (239) 430-3668 (FOOT) or visit www.NaplesPodiatrist.com to schedule an examination.
—–
Serving Southwest Florida Since 2005, Family Foot & Leg Center has multiple convenient locations throughout Collier, Lee, Charlotte, and Sarasota Counties. Offering pediatric to geriatric family care: Ingrown Toenails, Heel Pain, Bunions, Foot / Ankle Arthritis Pain, Plantar Fasciitis, Foot / Ankle Surgery, Custom Orthotics, and Diabetic Wound Care. In office X-rays, ultrasounds, and minor surgical suite exam rooms. Practice powered by EMR and advanced technologies.
Home of the Lam Minimally Invasive No-Scar Bunion Surgery! Come Discover Why Patients Love Our 5-Star Foot & Ankle Care!
For advanced wound management and diabetic wound healing resources, visit:
👉 WoundHealingExperts.com
Same Day Appointments! Easy Online Appointment Scheduling.

 Fax: (239) 692-9436
Fax: (239) 692-9436 Tel: 239-430-3668
Tel: 239-430-3668